
Table of Contents
Depression: The 3 Decades of the Prozac Paradox
In the late 1980s, a revolution swept through mental healthcare. In 1987, Prozac (fluoxetine) became the first Selective Serotonin Reuptake Inhibitor (SSRI) to be approved by the FDA for the treatment of clinical depression. When it was officially launched in 1988, it wasn’t just a new medication; it was a cultural phenomenon. It offered a seemingly simple solution—a chemical fix for what was largely believed to be a simple chemical imbalance. The numbers spoke for themselves: less than ten years later, Prozac achieved peak annual sales of an astounding $2.8 billion.
The market fervor and widespread adoption suggested a monumental public health problem had been solved. Yet, as we stand nearly three decades later, the reality is far more complex and sobering. Depression has not receded; it has become more persistent and widespread, a growing global public health crisis that continues to devastate lives and strain healthcare systems worldwide. This longevity of the problem forces a crucial question upon every consumer and clinician: If the breakthrough drug of the late 20th century was supposed to fix it, why is depression still rising, and what comes next?
The Core Challenge: Symptom vs. Root Cause
The fundamental issue lies in the mechanism of action. Standard SSRIs primarily function by increasing the availability of serotonin in the brain’s synapses. While this mechanism can be profoundly helpful for many individuals by alleviating the most severe symptoms—lifting the heavy fog, restoring some energy, and reducing suicidal ideation—it rarely addresses the core architecture of depression.
Antidepressants treat the symptom (the perceived chemical imbalance) but not the root cause. Depression is rarely just a serotonin deficiency. It is a complex disease often rooted in:
- Unresolved Trauma: Past adverse experiences that program the nervous system for threat and disconnection.
- Chronic Disconnection: Isolation from self, loved ones, community, and purpose.
- Destructive Lifestyle Factors: Chronic stress, poor diet, lack of physical movement, and poor sleep hygiene that dysregulate the body’s entire system.
- Cognitive Ruminations: Deeply ingrained negative thought patterns that sustain a depressive mood regardless of external chemicals.
By focusing solely on the chemical symptom, the underlying psychological, relational, and behavioral patterns that sustain depression remain untouched, making relapse common when medication is discontinued.
A New Frontier: The Psychedelic Renaissance
This systemic challenge has fueled a desperate search for therapeutic alternatives that can truly offer lasting change. Based on emerging clinical data and increasing medical interest, a completely different class of compounds is poised to enter the conversation: Psilocybin (found in “magic mushrooms”) and other psychedelics.
Initial trials show that Psilocybin, when administered in a medically supervised, therapeutic setting, can offer a profound shift in perspective that allows patients to break free from deeply entrenched negative thinking and emotional rigidity. While history may repeat itself in terms of market fervor and media excitement, the hopeful difference lies in the delivery system. Unlike taking a pill at home, effective psychedelic therapy requires an intensive, trauma-aware therapeutic framework—a structured approach involving preparation, the dosing session, and, crucially, post-session integration.
Beyond the Pill: Our Counseling-Coaching Commitment
This shift in focus—from passive symptom management to active inner transformation—is where our integrated counseling-coaching style steps in. We recognize that true recovery requires going beyond quick-fix chemical solutions.
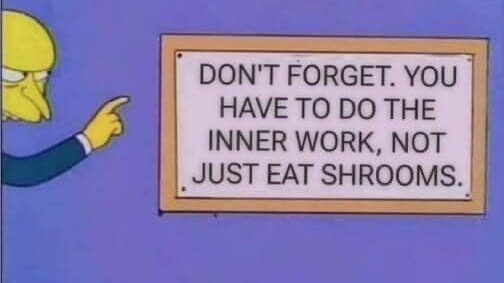
We work hard—we do the inner work—with our clients by focusing on:
- Exploring Root Causes: Utilizing deep counseling techniques to safely identify and process the past trauma, relational wounds, and self-limiting beliefs that created the depressive architecture.
- Developing Emotional Resilience: Teaching clients practical skills for self-regulation, mindfulness, and cognitive restructuring to manage high-stress moments without resorting to destructive coping mechanisms.
- Restructuring Life Habits: Employing life coaching strategies to systematically integrate positive behavioral changes—improving nutrition, sleep hygiene, and intentional social connection—that provide a foundational, chemical-free support system for the brain.
- Integrating Insights: For clients pursuing all forms of treatment, including novel ones, we provide the essential framework to integrate profound shifts or medication effects into stable, sustainable real-world behavior.
Our goal is simple: to help you achieve a robust and authentic sense of well-being that isn’t dependent on a continuous external chemical input. Our counseling-coaching style helps you be the best you by integrating both pharmacological understanding and deep psychological, relational, and behavioral healing.
Take the next step
Schedule a consultation to explore how counseling and coaching can support your journey toward well-being.

